Our Birth Story: Where Nothing Goes As We’d Planned

You can try and plan for everything, but it will never prepare you for everything. I am grateful and so very much in love with our beautiful boy Finley, but nothing could have prepared me for the adventure we had bringing this sweet being into the world.
I did more than just plan on having a quiet, natural home birth. I did absolutely everything within my means to ensure it. Not a single thing went according to plan.
I had done my research. I reluctantly read birth stories, not something I ever enjoyed, but was encouraged by some truly beautiful and peaceful birth stories. I also watched videos of beautiful births. This is not how my story goes.
This is the birth story of my baby boy Finley coming into this world, and of my husband Josh and I becoming parents.

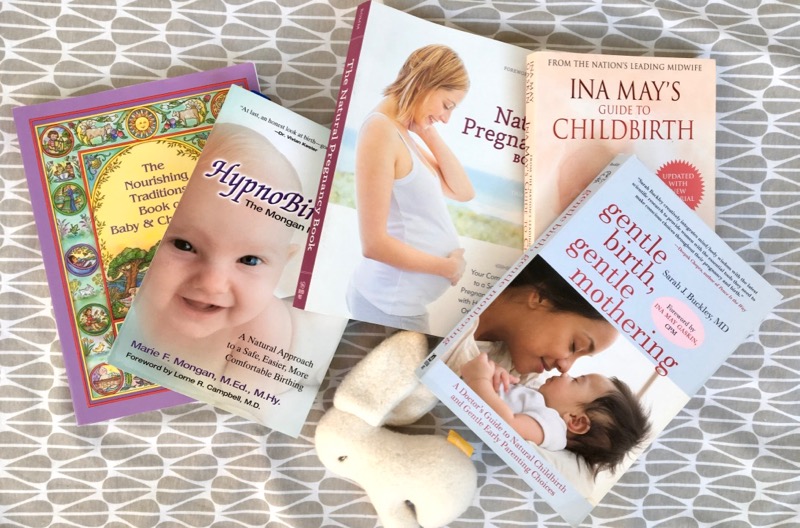
This photo and above by Catherine Farquharson
Preparing For My Natural Birth
Given my personal values and philosophy, I was keen on having a natural, home birth. It was the right choice for us, and more so, I believed it was the right choice for our baby. One of the first things my midwife said to me was that I was set-up for success. Natural births have become trendy, she explained, but most women who want a natural birth, aren’t living a fully natural, tuned in life. Our midwife and our doula both had full confidence that this would work for us.
When my first pregnancy ended in a miscarriage at 11+ weeks, I had my first lesson in the ways of pregnancy- that all I could do was my best, and the rest would be out of my hands.
I became pregnant nearly immediately after the miscarriage.
I had a text book pregnancy. All of the boxes were being checked off as I progressed week-by-week. The due date assigned by one of the two ultrasounds I got was June 7th. The due date I assigned based on knowing my cycle and conception time was June 12th. No problem, my midwife said, we’ll settle on June 10th and go from there.

June 7th came and went. June 10th, and then June 12th passed by and I became bigger and more uncomfortable than I thought possible. This was also when the first inkling of worry set in. I did not want intervention but as the pregnancy went into 41 weeks, and the baby still hadn’t dropped into my pelvis, I started to have some concerns. At the urging of my midwife, on June 19th (41 weeks and 5 days by the medical due date), I went for an ultrasound.
The ultrasound showed that my amniotic fluid was low and the technician measured the baby at 9+ lbs.
Research has shown that these two factors are not indicators of serious risk to the baby at this stage of pregnancy. Firstly, ultrasounds are notoriously inaccurate when it comes to measuring the size of a baby. When I looked into the implications of low amniotic fluid, the biggest risk factor listed was induction. This inferred that with low amniotic fluid, your greatest risk is not that the fluid is low (which can be caused by anything ranging from the position I am lying in, my hydration levels all the way to baby’s kidney function), but that your primary care provider will ring the alarm bells and push for an induction (loads of research is here).
I was not overly concerned by these two pieces of data. My midwife was.
I have defied conventional advice and experts in the past. That was how I healed from Crohn’s Disease. This time around, however, it wasn’t just my health or my life on the line. It was my baby that I was concerned about.
Up until this point I had absolutely no fear around labour and delivery. I had taken hypnobirthing classes, read loads of books, and talked with every woman I knew who had a natural birth. I had prepared my body with pelvic floor therapy, osteopathy, prenatal yoga, prenatal pilates, acupuncture, massage, optimal nutrition and more. I had truly progressed through this pregnancy shedding any fears as I went.
Once the results of that ultrasound came in, my midwife said it was time to start taking action to get this baby moving out. This was when fear started to set in.
Intervening On Nature
That evening, we went into the midwifery clinic and my midwife did a stretch and sweep, attempting to manually open the cervix before it was naturally primed and ready. This is considered a gentle way to stimulate labour. There was nothing gentle about it. Minor contractions began shortly thereafter.
Intervention had begun.
A doppler, an ultrasonic instrument for fetal monitoring that I had hoped not to have to use at all, was strapped on to me for 40 minutes to take a reading. After two hours at the clinic, I went home feeling bruised, battered and scared.
This wasn’t how it was supposed to unfold. Intervention wasn’t in my plans.
That evening, my acupuncturist came over and did nearly two hours of acupuncture and massage to try and stimulate labour. The goal was to further stimulate the uterus to contract as it had following the stretch and sweep, in hopes that labour would commence overnight.
My intuition had never been louder- The baby needs more time.
From the midwife’s exam, it seemed the baby’s head was turned slightly on an angle, preventing him from dropping into the pelvis. I immediately called my osteopath to find out what I could do to try and reposition the baby. I followed these exercises but feared I should have started this weeks earlier.
On Tuesday, we went in to meet with the midwife and, still not in labour, she recommended we plan to meet her at the hospital the following morning to be induced. This is when the fear started to suffocate me. Just like that the plans for a natural birth were dismissed.
I need more time, I told her. She did another stretch and sweep, this time stretching my cervix to 2-3 cm. At this point I was truly scared. I had given my power and confidence over to those with more experience than me and now all I could do was trust that they were right.
We agreed that if I did not go into labour overnight, I would try induction with castor oil.
Again, that evening, I had acupuncture at home. With contractions being more intense, Tanya worked on me for nearly three hours, until well past midnight when the surges petered out.
I slept well, woke up, drank a smoothie, and went for a long walk. It was time to drink the castor oil.
I am no stranger to cleansing, but castor oil had always been something I avoided due to how aggressive it is. I drank a shot of castor oil every 45 minutes. By mid-afternoon I was pooping oil and the cramping in my belly was beyond uncomfortable.
My midwife came to our house around 5:00pm to do another stretch and sweep, this time getting me to three centimeters. Within 30 minutes, I was in full-on labour.
Labour Begins
Ideally in labour, contractions start gently with a solid eight to ten minutes to recover in between. My contractions began at three minutes apart and they were doubling and tripling on each other. Before a contraction ended, another was beginning.
The next eight hours are a blur for me. Our doula arrived in the evening and her presence and massage through the intense contractions renewed my belief that I could do this. I tried taking a bath. I tried taking a shower. I rolled my hips on the ball. I walked. I lay down. I did everything I had learned. Nothing could ease the searing, life draining pain that shot through my body.
My water broke abut six hours into labour as my energy was waning and I started shaking violently. There was still oil leaking out of my body and with my contractions coming so close together, I couldn’t eat and could barely drink before another wave of pain would hit me.
The midwives showed up around midnight and did an exam. I was only four centimeters dilated. The baby wasn’t moving down. His head was still on an angle, they said.
At their urging, I tried walking up and down the stairs during contractions and doing deep lunges. I was exhausted, sweating and scared. All my confidence, my knowing that my body was made to do this, was gone. I didn’t know how I could go on. I didn’t think I could live through another contraction.
Looking back on these moments, these early morning hours that ticked by- every moment feeling like it would never end, it seems naive to think that dim lighting, a soundtrack of kirtan chanting and theta waves, some crystals and essential oils were going to help me. I wanted this to end. I needed this baby out of me.
Tossing Out The Birth Plan
Josh and I had spent a lot of time devising our birth intentions. We did deep research into every intervention, and knew what we were saying no to, and what would have to happen for any of them to get a yes.
- I did not want to go to the hospital.
- I did not want to be induced.
- I did not want pain medication.
- We wanted delayed cord clamping (not cord blood banking!)
- Oral vitamin K instead of the injection
- We did not want the erythromycin eye ointment.
- I didn’t want more people than essential in the room for the delivery.
- I wanted quiet and calm.
- I wanted immediate skin-to-skin.
I was so clear on these intentions that in the birth plan I wrote that if I asked for pain medication, to please talk me out of it. I had a greater fear of the cocktail of drugs being injected into my spine than I did the pain of labour. I felt comfortable and confident physically, emotionally and spiritually. I knew that the cascade of hormones in labour and birth were to work in my favour. I knew that oxytocin would help me through along with the support of my birth team- my husband, our doula and midwives. No one had any doubt that I was coming at this from the right place to ensure a successful home birth.
But the baby’s head wouldn’t budge and my cervix wouldn’t dilate. Now that I know my boy, I get it. He was just chilling.
Four hours after the first exam, and ten hours into labour, the midwives did another exam. I was now only five centimeters dilated. Our midwife gave me the option to try another two hours at home or transfer to the hospital.
Josh knelt beside me as I was shaking and writhing in pain. He told me I could do this. I knew with every fiber of my being that I could not. I have never been more sure of anything. I knew it was time to move.
He told me I could do this. I knew with every fiber of my being that I could not.
Transfering To The Hospital
Preparing to leave for the hospital was a blur. We walked out of our house into the pre-dawn morning as the sun was beginning to rise. The fifteen minute drive to the hospital felt like a lifetime. I was dropped off at the emergency entrance, moved into a wheel chair and was swiftly wheeled up to the labour and delivery wing of Mt. Sinai hospital.
Upon entering the room, I was changed into a hospital gown. I have a vague memory of the anesthesiologist reviewing the potential side effects of the epidural. Pain. Headache. Paralysis. Death. I agreed that I understood the risks. I felt the pinch in my back. Within moments, sweet relief overcame me. I could breathe again.
With all my being I wanted a natural birth. I wanted all the benefits, and wanted minimal interventions, not just for my benefit but moreso for my baby. It was my baby I was most concerned about.
I was on an IV of Pitocin (synthetic oxytocin), an anesthetic and a saline solution. In front of me, was a giant clock and I watched the hours tick by. I remember thinking how very long this day was. I thought about my team at work and what they would be doing. I fell in and out of an exhausted sleep. My midwifery team had a change over so my primary care team could go home and sleep. My husband and doula stayed by my side. My mom arrived at some point. I had a midwife monitoring my vitals. There was constant fetal monitoring.
Every few hours the obstetrician on duty came in to check on me. I was dilating about one centimeter every two hours.
Would This All End With A C-Section?
The first signs of meconium showed around 2pm. It had leaked out of me with the contractions. The risk was that the baby could aspirate the meconium and go into distress. My midwife had mentioned this as a risk of going past the due date and of long labour, but had said this had happened only once in her fifteen years of practice.
At 4:00pm, my midwife explained what would happen with a c-section, that I would be transferred to another room, be given an IV of antibiotics, and more anesthetic. I was told what would happen after the baby was delivered. I was overcome with fear and when I looked over at Josh, I saw the tears in his eyes.
And still we waited.
Let’s Bring This Baby Into The World!
At 7:20pm the obstetrician came in to examine me. At twenty-five hours into my labour, I was 9 1/2 centimeters dilated and she said I could try pushing to see what what would happen. I had one push to determine whether I could continue with a vaginal birth. I felt nothing from the waist down. I didn’t feel any contractions. I couldn’t feel an urge to push.
About a dozen people poured into the room, the OB, her students, and a resuscitation team. The bright lights came on over me, and I also noticed the lights go on over in the corner for the infant resuscitation table.
It was time to bring my baby into the world in every way I had hoped for it not to happen.
I had been taught ways to breathe the baby down, and to wait for the body’s natural inclination to push. Instead I pushed in all the ways I had been instructed not to. This was what is commonly referred to as purple pushing. My legs were being held up by my doula and my husband, and a blur of people around me shouting push, push, push.
We need you to push again, the doctor told me, so we can position the baby’s head for the vacuum or forceps.
I didn’t want either. Pushing this baby out, was the only thing left on my birth plan. On the next contraction, I pushed again. I couldn’t feel anything. I looked at the clock. 7:26pm. I had pushed so well, that we were good. No further intervention was needed. I just had to get this baby out fast. There was more meconium and I could tell there was some concern.
With each contraction I pushed. They could see the head, all the hair of our little babe. Still I couldn’t feel anything. I was numbed by the drugs and by exhaustion. I looked at the clock. 7:40pm.
One final push and the baby arrived.
Seven pounds, four ounces, born at 7:42pm on Thursday, June 22nd.
That Was The Easy Part
After 25 hours of labour, where nothing went according to plan, a nightmare slowly began to unfold.
The baby came out limp and blue. I knew it often took a moment for a baby to cry, so I wasn’t too concerned. There was a long pause, looks around. Someone said, It’s a boy!
Josh was urged to cut the cord. We wanted to delay clamping, he explained.
There isn’t time, was the response. I was ready to receive my baby, to lay him on my abdomen and let him find my breast, and to nurse skin-to-skin.
Instead he was rapidly transferred to the resuscitation team. He had aspirated meconium and wasn’t breathing. He was intubated, his lungs were pumped, and I kept waiting for an answer to my question, Is he okay?
The baby boy was wrapped in flannels and I was able to hold him for a minute or two before he was whisked away to the resuscitation room. Josh followed them out.
By this time my dad and my mother-in-law had arrived . We were all celebrating the arrival of our baby boy, but the baby wasn’t there. I didn’t know what was happening. I kept waiting for them to bring him back.
His First 24 Hours Of Life
I was transferred into a shared room in the maternity ward. The basinet the baby was meant to sleep in was quickly wheeled out. The order of events that followed is blurry for me. I was told that our baby had been transferred to the neonatal intensive care unit. The fire alarm was going off in the hospital, a siren blaring every few moments. You could hear the cry of all the newborns, but not mine.
Through the blaring of the fire alarm and my exhausted haze, the doctors attempted to explain what had happened and what was happening. Our baby was going for a chest x-ray. He was being given antibiotics. They were running blood tests. He was having trouble breathing. Soon I could go up and see him.
Josh wheeled me up to the NICU, as I began to disconnect from this reality. I was seeing all the babies in their incubators, connected to machines. One of them was mine.

I cried for our little man, who was in such distress, his chest heaving as he tried to breathe. There were tubes up his nose, monitors on his chest and an IV in his hand. And I cried because he didn’t feel like mine. It was now midnight. I moved into a chair and they took the baby out of his incubator and put him on my chest. He cried and I cried. I didn’t know what to do.
I couldn’t nurse him because his breathing was so intense, they were afraid he might choke. I didn’t know how to comfort this baby.
Josh and I spent that night in the shared room in the maternity ward, being woken by the cries of other people’s babies.
In the baby’s first 24 hours of life, I was able to hold him for a few moments at a time. He underwent three chest x-rays, numerous blood tests and ultimately ended up on two different antibiotics, along with a fluorescent yellow IV of dextrose.
I had no choice but to zip my mind up.
I couldn’t think about all of the needles, and x-rays, or the antibiotics being the first thing to enter his fragile system. I couldn’t think about him getting fluorescent yellow corn-based sugar water as his first food, or the constant glow of fluorescent lights, lack of fresh air, persistent beeping of the machines, immediate use of a pacifier, the hand sanitizer being doused on the hands of every nurse and doctor before they entered his room, the WiFi router blinking it’s blue light directly over his incubator, or the petroleum jelly they were using on his bottom.
This couldn’t have been further from what I had imagined his entry into the world would be.

All I could do was hope and pray that he would be okay, that he would recover, that he would survive this. No one could tell me that.
On Saturday morning I was discharged from the maternity ward while our baby was undergoing a spinal tap. His blood work had shown elevated levels of inflammatory markers and there was concern of a secondary infection or meningitis.
One Week In The Neonatal Intensive Care Unit
I was moved into a “nursing mother’s” room. It was a tiny closet of a room, just large enough for a single bed and the shared bathroom was across the hall. Everything about this felt wrong. I had just given birth to my baby and here I was in this room alone, with my baby too far for me to walk to him on my own.
On Saturday afternoon I was given the go-ahead to try nursing. Any first time nursing mother knows it’s not that simple. It didn’t help that he’d been sucking on a pacifier since the moment of birth and that his hunger was being soothed with intravenous sugar water. He just cried.
That evening I connected with a lactation consultant. She graciously agreed to come to the hospital Sunday morning to help me get the baby to nurse. The NICU rules don’t permit anyone aside from the parents to hold the baby, so Taya stood beside us, and offered direction. Within 15 minutes the baby was latched and hungrily nursing away. By 12:00pm his IV was decreased, and by 4:00pm he was off completely, receiving 100% of his nourishment from me.
At last, on Monday we received good news. His cultured blood work came back clear. Despite there being no sign of infection, the baby had to continue on his course of antibiotics.
I spent the next three nights in the nursing mother’s room. The nurse on duty would call me every two hours throughout the night to come feed the baby. Josh was with me from first thing in the morning until I went to sleep.
Our baby continued to improve through the week. He grew stronger, his colour changed, his smell changed, and his poops changed. His cry got louder and he nursed with more urgency.
A few nights later, I was moved into a new room, where there was space for Josh to stay over with me. And on our final night in the hospital, our baby was detached from the machines and permitted to stay in the room with us.

It wasn’t until Thursday, a full week after his arrival, when I signed the discharge papers for our baby, that I could truly accept and celebrate that our baby had arrived. He was here, he was safe, and it was time to take him home.

So It Wasn’t A Natural Birth. That’s Not The Part That Keeps Me Up At Night
Throughout the time of early labour, through to our discharge from the hospital, I couldn’t think too hard about what was happening. If I started to, I don’t know that I could have coped. There were definitely moments in the shared bathroom, as I was showering and brushing my teeth that I grieved the calm, quiet bonding time I had envisioned at home. I got over that, though. All that mattered for that week was that our boy was getting better.
I left the hospital so incredibly grateful to all of the doctors and nurses that saved the life of my baby, and I do believe, my own life too. I am beyond grateful to live in a country that provides the medical care we received as part of being a citizen of this country.
I have had people ask me since the birth of our son, how I feel about the birth and the fact that it was not at home, not natural and as far as possible from what we planned. In complete and total honesty, I don’t care at all. Having a natural birth was my choice because it felt like the right one through and through. I know that once labour began, I did everything that I could to ensure the safety of our baby. I don’t stay up at night imagining what the birth could have been. I don’t feel remotely guilty or regretful.
There are questions I asked in the days following our boy’s arrival. Did my determination to have a vaginal birth put him at greater risk? Would he have been better off with a c-section delivery once we saw the meconium? Would that have spared him all of the interventions that followed? Should I have skipped the castor oil, and opted for a medical induction? Should I have insisted on one more ultrasound before intervening at all?
These aren’t the questions that haunt me.
There is a bigger what if that I will live with the rest of my life. What if I had trusted my instinct? It’s not time. The baby just needs more time. He’s not ready. This is the thought that keeps me up at night.
Post traumatic stress disorder is not uncommon following births that don’t go as planned. People will say to you, It’s okay, you have a healthy and happy boy. Everything is fine now.
I am overjoyed, and truly overwhelmed with gratitude that Finley recovered fully. As I write this he is a thriving, incredibly healthy, calm, smiley, and very chubby 3-month old. This fact does not undo what I went through. It can’t erase the emotional, physical and spiritual memory. It doesn’t undo the trauma that was experienced. People will say to me that you forget. That I’ll forget. I don’t think I ever could, nor would I want to.

 Photos by Catherine Farquharson
Photos by Catherine Farquharson
Thinking about the days in the hospital are harder now, than they were to live. Now I know Finn. Now, he is my son. Now he feels like my son.
There are so many factors, so many variables to consider as we decide how to bring our children into the world and how to best raise them. Though I continue to wonder what would have happened if only I had trusted my intuition, I am also coming to realize this is the mind of a mom and a dad. There can always be more what ifs.
I continue to work through and process our family’s birth experience. There is no point in ever looking back at our choices with what ifs. It can make us crazy. As parents, I do believe, it is our responsibility to simply make the best decisions we can in the moment, with what we know and what we feel to be right.
Yes, I had planned for a natural birth. I was the perfect candidate for such a birth. I ate right, did all of the physical therapies to prepare my physical body and spent a lot of time meditating, reading, walking and spending time in silence to mentally and emotionally prepare. I have no doubt that, even though all of my preparation wasn’t used for my natural birth, it was invaluable in my recovery. My physical body recovered remarkably well, and for ever bit of time and energy and effort I put into preparing for birth, I am forever grateful. It meant that I had the physical and mental ability to cope with the days and weeks that followed our traumatic birth.
This isn’t an easy story to tell, but it needs to be told because I know I am not the only one. After Finn’s birth, so many women reached out to me with their traumatic birth stories. It’s okay. Our stories have their own beauty, much of that beauty coming in the form of the strength these early challenges have given to us as women and as mothers.
We are foolish to think we can control how our lives, and the moments that make up our lives unfold. All we can ever control is how we choose to respond in any given moment. Right now, I am choosing love, gratitude and presence with my baby boy.
Free Resource Library
Enjoy more than 40 downloadable guides, recipes, and resources.















 Photos by Catherine Farquharson
Photos by Catherine Farquharson